Now that you’ve learned what the lack of vitamin B12 causes, and about the symptoms of low B12, we’ll now see what exactly causes vitamin B12 deficiency in the first place. There could be a few reasons, and each of them demands an immediate treatment.
Vitamin B12 Deficiency Causes
So, what causes low B12? Let’s start.
Low B12 Intake
The most obvious cause of B12 deficiency is low dietary intake. Vegans and vegetarians are especially at high risk, together with their infants and children:
Higher rates of deficiency were reported among vegans compared with vegetarians and among individuals who had adhered to a vegetarian diet since birth compared with those who had adopted such a diet later in life. The main finding of this review is that vegetarians develop B12 depletion or deficiency regardless of demographic characteristics, place of residency, age, or type of vegetarian diet. Vegetarians should thus take preventive measures to ensure adequate intake of this vitamin, including regular consumption of supplements containing B12.
HOW PREVALENT IS VITAMIN B(12) DEFICIENCY AMONG VEGETARIANS?

There are no reliable vegan sources of B12, and no vegetarian or vegan should live without regular B12 supplementation. Even the Vegan Society supports this. Infants born to mothers who were deficient prior to conception or during their pregnancy or nursing may end up deficient themselves. Unlike adults, they have no stores of B12. Low B12 causes developmental issues, and such babies should start B12 therapy immediately. The effects of B12 deficiency on children raised vegan are especially scary:
… a significant association between cobalamin [b12] status and performance on tests measuring fluid intelligence, spatial ability and short-term memory with formerly vegan kids scoring lower than omnivorous kids in each case … reasoning, the capacity to solve complex problems, abstract thinking ability and the ability to learn. Any defect in this area may have far-reaching consequences for individual functioning.
Signs of impaired cognitive function in adolescents with marginal cobalamin status
Other demographics with low B12 intake may be anorexic or bulimic people, or the underprivileged who just can’t afford B12-rich animal foods (common in Third World countries). Some people also have increased demands, such as those with chronic hemolytic anemia, multiple myeloma, hyperthyroidism, myeloproliferative disorders, neoplasms, and pregnant women. These are all risk groups for B12 deficiency.
Impaired Absorption
Most B12 deficiencies have nothing to do with low intake, but everything to do malabsorption. The main reasons for B12 deficiency are pernicious anemia (caused by antibodies), and food-cobalamin malabsorption (caused by achlorhydria or H.pylori gastritis, certain medicines, or the surgical removal of any part of the stomach):
Cobalamin (vitamin B12) deficiency is particularly common in the elderly (>65 years of age), but is often unrecognized because of its subtle clinical manifestations; although they can be potentially serious, particularly from a neuropsychiatric and hematological perspective. In the general population, the main causes of cobalamin deficiency are pernicious anemia and food-cobalamin malabsorption. Food-cobalamin malabsorption syndrome, which has only recently been identified, is a disorder characterized by the inability to release cobalamin from food or its binding proteins. This syndrome is usually caused by atrophic gastritis, related or unrelated to Helicobacter pylori infection, and long-term ingestion of antacids and biguanides.
An update on cobalamin deficiency in adults
In PA, antibodies prevent the body from creating intrinsic factor, a protein needed for the absorption of B12. It is a more complete type of malabsorption, where B12 injections are needed to protect patients from severe nerve and brain damage. On the other hand, in food-cobalamin malabsorption, the body is unable to release the B12 from food, though it can still fully absorb the free crystalline form found in oral supplements or fortified foods. Food-cobalamin malabsorption is the more common type in the elderly:
Low cobalamin concentrations are common in the elderly. Although only a minority of such persons display clinically obvious symptoms or signs, metabolic data clearly show cellular deficiency of cobalamin in most cases. The evidence suggests that this is not a normal physiologic expression of the aging process. Rather, the elderly seem at increased risk for mild, preclinical cobalamin deficiency. Classical disorders such as pernicious anemia are the cause of this deficiency in only a small proportion of the elderly. A more frequent problem is food-cobalamin malabsorption, which usually arises from atrophic gastritis and hypochlorhydria but other mechanisms seem to be involved in some patients. The diminished absorption should not be viewed as a natural consequence of aging. The partial nature of this form of malabsorption produces a more slowly progressive depletion of cobalamin than does the more complete malabsorption engendered by disruption of intrinsic factor-mediated absorption. The slower progression of depletion probably explains why mild, preclinical deficiency is associated with food-cobalamin malabsorption more often than with pernicious anemia.
Cobalamin, the stomach, and aging
Vitamin B12 or cobalamin deficiency occurs frequently (> 20%) among elderly people, but it is often unrecognized because the clinical manifestations are subtle; they are also potentially serious, particularly from a neuropsychiatric and hematological perspective. Causes of the deficiency include, most frequently, food-cobalamin malabsorption syndrome (> 60% of all cases), pernicious anemia (15%-20% of all cases), insufficient dietary intake and malabsorption. Food-cobalamin malabsorption, which has only recently been identified as a significant cause of cobalamin deficiency among elderly people, is characterized by the inability to release cobalamin from food or a deficiency of intestinal cobalamin transport proteins or both.
Vitamin B12 (cobalamin) deficiency in elderly patients
Older adults who’ve had surgical removals of parts of their stomach (such as in weight-loss surgeries, certain types of cancer, or the outdated antrectomy or vagotomy procedures), should also be concerned:
Patients undergoing bariatric surgery must be continuously educated on proper nutrition, the risk of developing significant vitamin B12 deficiency, and the role of supplements in avoiding catastrophic consequences.
Vitamin B12 deficiency in patients undergoing bariatric surgery: preventive strategies and key recommendations
But that’s not all.
What else can cause B12 malabsorption?
The impaired absorption of B12 can also arise from the pancreas, where the enzyme that frees the B12 from its complex is absent or inhibited. Cystic fibrosis, chronic alcoholism, Zollinger-Ellison syndrome, and pancreatic cancer are all examples of possible contributors. There’s also a rare genetic disorder called mucolipidosis type IV that can cause malabsorption by lowering acid production in the stomach.
Also, problems in the small intestine could lead to malabsorption, because it is where the B12-intrinsic factor complex is absorbed. That’s where it is freed before it can attach to transcobalamin-II, to be circulated in the blood for our various organs to use.
In celiac disease, for example, the lining of the ileum is damaged and cannot take up B12. In Crohn’s disease, the immune system attacks the gastrointestinal tract, affecting literally all of its parts. Surgical removal of the ileum is another obvious example.
Competing Creatures
Another possible reason for vitamin B12 deficiency is a parasite infestation, or bacterial overgrowth. For example, some worms may make their way into our intestines and take up nutrients from our foods, effectively competing with our gut for B12. One example is fish tapeworm, found around Canada and Alaska. Gastrointestinal parasitic infestation – like giardiasis, caused by the microscopic parasite Giardia – can behave similarly.
Overgrowth of the normally present bacteria in the gut may also lead to vitamin B12 deficiency. If your normal gut flora overgrowths, it will start consuming your B12. Bacterial overgrowth may be the result of disease like diverticulosis, where sac-like dilatations form in the gut, with bacteria accumulating there.
The Depletion of Available B12
Some drugs interact with B12 and decrease its levels, either by inhibiting its availability (malabsorption issues, as mentioned above), or by causing a greater excretion. The most famous suspect is metformin, a drug used widely for the management of diabetes. According to reports, about 30% of the patients taking this drug for a prolonged period of time eventually develop a B12 deficiency. According to one study:
Long-term use of metformin in DPPOS was associated with biochemical B12 deficiency and anemia. Routine testing of vitamin B12 levels in metformin-treated patients should be considered.
Long-term Metformin Use and Vitamin B12 Deficiency in the Diabetes Prevention Program Outcomes Study
Other suspect drugs are salicylates (aspirin), anti-tuberculosis drug isoniazid, epilepsy drugs phenobarbital, pheytoin & primidone, gout drug colchicine, AIDS drug zidovudine, and drugs that lower the acidity of the stomach (like those given to patients with reflux disease). B12 supplementation in all these patients is necessary.
Also, anyone on B12 deficiency treatment should not be given certain antibiotics (those of the aminoglycoside group, like gentamicin and tobramycin).
What else causes B12 deficiency due to depletion?
Toxins.
One of the various benefits of B12 is that it helps remove toxins from our body. For instance, alcohol is a toxin, and for that reason chronic alcoholism significantly reduces B12 levels in the blood. Another common toxin that does no good to your B12 stores is cyanide (from cigarettes, etc), which B12 helps clear out of your system.
Another example is nitrous oxide (N20, or ‘laughing gas’), which irreversibly oxidizes the cobalt ion of the B12 from its active state to an inactive state, rendering it useless to the body. The use of N20 (either as anesthesia, or as ‘hippy crack’) can be devastating:
Nitrous oxide produces irreversible oxidation to the Co++ and Co forms that renders vitamin B12 inactive. Five cases (four from the literature and one new case) are presented in which patients unsuspected of having vitamin B12 deficiency developed subacute combined degeneration of the spinal cord following nitrous oxide anesthesia. Patients with vitamin B12 deficiency are exceedingly sensitive to neurologic deterioration following nitrous oxide anesthesia. If unrecognized, the neurologic deterioration becomes irreversible and may result in death.
Neurologic degeneration associated with nitrous oxide anesthesia in patients with vitamin B12 deficiency
Phillip Lee and colleagues (March 13, p 554) highlight the danger of giving nitrous oxide to patients who may have unrecognised vitamin B12 deficiency. The number of patients reported to develop neurological problems is now into double figures. However, the worrying aspect of this report, from an anaesthetist’s point of view, is that nitrous oxide was given for only 65 min. Since many operations last considerably longer than 1 h the implication is that are are putting a substantial number of patients at risk.
Vitamin B12 deficiency and nitrous oxide
Given the scale of use which would result from routine use of nitrous oxide in children undergoing painful procedures, there should be real concern about the potential for an accident in a child with occult cobalamin deficiency. The message must be: never forget vitamin B12 when thinking of using nitrous oxide.
Nitrous oxide and vitamin B12
Genetic Causes of B12 Deficiency
There are also genetic causes. If genes responsible for B12 metabolism were affected, absorption of B12 could be hampered. Eight such genes have been found so far:
To function as a cofactor, B12 must be metabolised through a complex pathway that modifies its structure and takes it through subcellular compartments of the cell. Through the study of inherited disorders of vitamin B12 utilisation, the genes for eight complementation groups have been identified, leading to the determination of the general structure of vitamin B12 processing and providing methods for carrier testing, prenatal diagnosis and approaches to treatment.
Genetic disorders of vitamin B12 metabolism: eight complementation groups – eight genes
Mutations in genes encoding endocytic receptors involved in the ileal absorption and cellular uptake of cobalamin have been recently uncovered and explain, at least in part, the hereditary component of megaloblastic anemia.
An update on cobalamin deficiency in adults
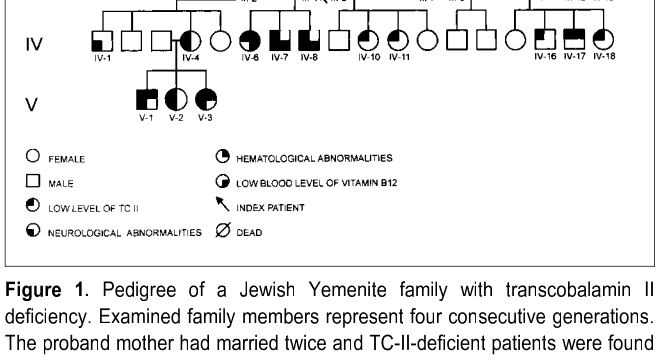
Examples would be babies born with congenital pernicious anemia, in which their bodies can’t produce the intrinsic factor they need to absorb B12. This is an inherited disorder with disastrous outcomes if not treated with B12 shots immediately. Other disorders would be hereditary TC-II deficiency, or Imerslund–Gräsbeck syndrome.
Summary
B12 deficiency could be the result of one of these:
- Low dietary intake.
- Impaired absorption.
- Bacteria or parasites competing for it.
- Depletion by toxins or drugs.
- Genetic disorders.
Now that you know what causes low vitamin B12, it’s time to learn how exactly you should treat a B12 deficiency, and which supplement is best for you.
All the best.