There are four forms of vitamin B12. Which one is best for you?
First, some background.
Vitamin B12, also known as cobalamin, is the largest and most complex vitamin out there. It is unique because it is the only vitamin that contains a metal ion, cobalt (hence its name). It is also a co-factor for two enzymes in mammals (and you are a mammal) – one is methionine synthase, the other is methylmalonyl-CoA mutase.
The molecule that is attached to the cobalamin is called a donor. The two most common donors in supplements are cyanide (making the type of B12 known as cyanocobalamin, or cyano B12) and methyl (making what’s known as methylcobalamin, or methyl B12). Two other forms you may find are hydroxocobalamin and adenosylcobalamin.
These forms of vitamin B12 are all present to some degree in the foods you eat, with the predominant ones being adenosylcobalamin and hydroxocobalamin. Another B12 form found in foods is sulphitocobalamin. We won’t cover it here because it’s irrelevant, as you will never find any supplements made from that form – they do not exist.
Only adenosylcobalamin and methylcobalamin are active within our bodies. You’ll find methyl B12 in the blood plasma, cytosol cells, and certain fluids (like cerebral spinal fluid), and adenosyl B12 in cellular tissues, stored in the mitochondria.
In fact, the benefits of B12 boil down to two biochemical reactions. First, the conversion of methylmalonyl-coenzyme A to succinylcholine coenzyme A, by methylmalonyl-CoA mutase, with adenosyl B12 as a co-factor. Second, the remethylation of homocysteine to methionine, by methionine synthase, with methyl B12 as a co-factor.
Not to complicate things any further, let’s get back to our question:
Which type of B12 should you supplement with?
Best Forms of Vitamin B12: Methylcobalamin vs Cyanocobalamin vs Hydroxocobalamin vs Adenosylcobalamin
Let’s explore all forms of vitamin B12, one by one.
Cyanocobalamin
(Also known as CN-Cbl or Cyano B12)
Cyano B12 is a cheap, synthetic, slightly toxic, inactive form of B12 that is made with a cyanide donor and is used commercially. It’s the most stable form, because the cyanide molecule has the greatest attraction to the cobalamin, thus protecting it from conditions like high temperatures. Cyano B12, however, doesn’t absorb well and requires a methyl group to detoxify it before it can ever convert to a useful form.
When cyano B12 does absorb, it converts to hydroxo B12 (hopefully discarding the cyanide in the process). Then, it converts to methyl B12 and adenosyl B12. Taken orally, cyano B12 absorption is drastically reduced if you have any gastric acid issues.
We can’t recommend this form to anyone.
Sure it’s cheap, but it comes with a hidden price. Again, before it can be converted to an active form that you can use and absorb, your body must use a methylation reaction to cleave the cyanide out. This decyanation process is demanding:
Although the amount of cyanide is considered toxicologically insignificant, humans must remove and detoxify the cyanide molecule, reduce the cobalamin to its usable +1 oxidation state, and then enzymatically convert the cobalamin into one of two metabolically active coenzyme forms. Nutritional inadequacies, enzyme defects, and pathological changes to tissues can all contribute to a reduced ability of the body to accomplish the synthesis of the active forms of vitamin B12 from CN-Cbl.
The Coenzyme Forms of Vitamin B12
Methylation is one way through which your body detoxifies. But it requires methyl molecules, which are often in low supply (modern life is full of toxins), especially in folks suffering from B12 deficiency or pernicious anemia. This is why people with methylation issues (like autistic children) can get worse on CN-Cbl but not on other forms of B12.
Then why does cyano B12 even exist?
Commercial cyano B12 exists because, when making hydroxo B12 from bacteria, some of the cobalamin binds to cyanide during the charcoal filtration process.
Check out this paper from 1992:
If the indiscriminate dumping of industrial cyanide waste continues unchecked with the inherent risk of pollution of food and water supplies there may well come a time when more widespread chronic cyanide neurotoxicity occurs in the Western hemisphere from a dietary source in persons with a genetic or acquired error of cyanide or vitamin B12 metabolism.
Cyanocobalamin- a case for withdrawal: discussion paper
We all get cyanide into our systems – pollution, barbecue, bonfire, secondhand smoke, even almonds. The body always has to detoxify it. By taking cyano B12, you’re further depriving your body of methyl groups, a natural antidote, an antagonist for toxins.
Because of this detoxification process, cyano B12 could potentially deplete glutathione (GSH), an important antioxidant that helps decrease lipid peroxidation associated with oxidative stress. Once glutathione stores are empty, high-dose cyanocobalamin may theoretically cause cyanide toxicity, especially in renal failure patients.
Also, some people may have conditions that inhibit them from converting this form of B12 into the active forms that you can absorb. In these cases, serum B12 levels will shoot up (the blood test counts inactive B12 too), but there may still be a deficiency of adenosyl B12 and methyl B12 in the cells, tissues and body fluids.
It takes more than 48 hours for cyano B12 to convert to usable methyl B12. Even then, only a small amount is converted. Remember, in this conversion process, it requires the interaction – possibly the depletion – of glutathione and other agents. For that reason, it can make Leber’s optic atrophy worse, and nobody should ever use it in that case.
Why can you even buy cyano B12 then?
Despite all the above, cyano B12 is the most prescribed form. Reason? It’s cheap. But it’s also the least safe, least effective, and most demanding type of B12.
Not natural to mammals whatsoever.
Why would you try to improve your health with something that requires the depletion of other crucial substances? It makes no sense, especially when there are other, much better forms of vitamin B12 that don’t cost much at all.
Methylcobalamin
(Also known as Mecobalamin, MeCbl, MetCbl, MetB12, MeB12, or Methyl B12)
Methylcobalamin as an endogenous coenzyme plays as important a role in transmethylation of methionine synthetase in the synthesis of methionine from homocysteine. It is transported to nerve cell organelles, and promotes nucleic acid and protein synthesis. Transportation of methylcobalamin to nerve cell organelles is better than both hydroxocobalamin and cyanocobalamin. It is involved in the synthesis of thymidine from deoxyuridine, promotion of deposited folate utilisation and metabolism of nucleic acid. It promotes nucleic acid and protein synthesis more than adenosylcobalamin does. Methylcobalamin promotes axonal transport and axonal regeneration. Methylcobalamin normalises axonal skeletal protein transport in nerve cells in animal models of diabetes mellitus. It exhibits neuropathological and electrophysiological protective effect on nerve degeneration in animal models of axonal degeneration (adriamycin, acrylamide, and vincristine-induced neuropathies) with spontaneous diabetes mellitus. It promotes myelination (phospholipid synthesis). Methylcobalamin promotes the synthesis of lecithin, the main constituent of medullary sheath lipids, and increases myelination of neurons in tissue culture, more than adenosylcobalamin does. It restores delayed synaptic transmission and diminished neurotransmitters to normal.
Oxford Biosciences
Methylcobalamin is one of the two active forms of vitamin B12. It reduces homocysteine and generates SAMe (S-adenosyl methionine), the most crucial methyl donor we have. In other words, it supplies methyl groups for the crucial chemical reactions we discussed.
Where methyl B12 shows its greatest utility is with people suffering from degenerative neurological symptoms, where it’s often the only promising treatment. It bypasses several potential issues in the absorption cycle and helps relieve or reverse symptoms. It is the best form to help regenerate nerves and treat peripheral neuropathies.
High doses of methyl B12 have been used to treat amytropic lateral sclerosis and Parkinson’s. It also improves visual and auditory symptoms in multiple sclerosis, and it improves memory and intellectual function in Alzheimer’s patients.
Is methyl B12 really so effective? Is it the best type of B12?
In fact, it is so effective that Japan uses it almost exclusively to treat B12 deficiency. Of all vitamin B12 forms, the science on methyl B12 is the most astounding:
It may dramatically improve recovery for facial nerve function in Bell’s palsy patients. In high doses, it may promote neuronal function, nerve regeneration, and even protect cortical neurons against neurotoxicity. In diabetic neuropathy, it may improve burning sensations, numbness, loss of sensation, muscle cramps, reflexes, lower motor neuron weakness, and sensitivity to pain. If you combine the methyl B12 with ginkgo biloba, or L-methylfolate and pyridoxal 5′-phosphate, improvements may be even better.
One study induced hemolytic hyperchromic anemia and impairment of hematopoiesis in the bone marrow of rabbits, and a decrease in blood-serum methylcobalamin was observed. Methyl B12 administration then fully normalized some hematopoiesis and blood patterns, improved the ratio between the B12 forms, and completely regenerated total B12 content. Adenosyl B12, the other active form, showed a much lower effect.
What else?
In both in-vitro and in-vivo experiments, methylcobalamin inhibited the proliferation of malignant cancerous cells. Paired with adenosyl B12, it reduced tumor growth and enhanced survival time of mice with Ehrlich ascites tumor cells. It also increased survival time of leukemic mice, whereas cyano B12 was inactive under the same conditions. Evidence suggests that it may also enhance the efficacy of methotrexate.
And there’s more:
Chronic administration of methyl B12 was shown to protect cultured retinal neurons against N-methyl-D-aspartate-receptor-mediated glutamate neurotoxicity. It may also improve deteriorated accommodation following visual work. Methyl B12 produces improvements in several components of heart rate variability, suggesting a balancing effect on the sympathetic and parasympathetic nervous systems.
As you see, methyl B12’s applications are endless
Under experimental conditions, methyl B12 (adenosyl and hydroxo B12 as well, actually) inhibited HIV-1 infection of normal human blood lymphocytes and monocytes.
In one study, daily doses of 6,000μg of methyl B12 for four months improved sperm count by 37.5%. In another study, daily doses of 1,500μg for 4 to 24 weeks increased sperm concentrations in 38% of all cases, total sperm count in 54% of all cases, and sperm motility in 50% of all cases. This is incredible.
One study reported a case of a 48 year-old woman with motor weakness, dementia, sensory disturbances, and widespread coarse hair – classic B12 deficiency symptoms. In response to methyl B12 shots (500μg every other day), her weird sensations resolved, dementia was reduced, hand grip strengthened, hair texture normalized, and she was now able to walk on tiptoe. Results like this are not by any means rare.
Also, remember we talked about B12 converting homocysteine to methionine?
This is specfically the job of methylcobalamin, and it’s why high levels of homocysteine can be a sign of low methyl B12 levels. In one study, high homocysteine levels went from 14.7 down to 10.2 nmol/ml following methyl B12 shots. Thanks to this profound effect, methyl B12 is our favorite form of B12. It is also useful in children with autism, and in reducing cognitive decline and cardiovascular outcomes in older patients.
On methyl B12 and sleep
The science on methyl B12 and sleep is really promising. We don’t fully understand how, but it seems like this type of B12 could modulate the synthesis of melatonin, a hormone involved in regulating your sleep-wake cycle:
Eight young males were subjected to a single blind cross-over test to see the effects of vitamin B12 (methylcobalamin) on the phase-response of the circadian melatonin rhythm to a single bright light exposure. VB12 (0.5 mg/day) or vehicle was injected intravenously at 12:30 h for 11 days, which was followed by oral administration (2 mg x 3/day) for 7 days. A serial blood sampling was performed under dim light condition (less than 200 lx) and plasma melatonin rhythm was determined before and after a single bright light exposure (2500 lx for 3 h) at 07:00 h. The melatonin rhythm before the light exposure showed a smaller amplitude in the VB12 trial than in the placebo. The light exposure phase-advanced the melatonin rhythm significantly in the VB12 trail, but not in the placebo. These findings indicate that VB12 enhances the light-induced phase-shift in the human circadian rhythm.
Vitamin B12 enhances the phase-response of circadian melatonin rhythm to a single bright light exposure in humans
It makes sense, because the formation of melatonin requires a methyl group. Another study reported that methyl B12 improved alertness and increased rectal temperature in later daytime hours. This suggests that B12 indeed affects the circadian clock.
One study tested the effects of methyl and cyano B12 on circadian rhythms, well-being, alertness, and concentration in healthy subjects. Sleep time was significantly lower in the methyl B12 group, who reported better sleep quality, focus, and a refreshed feel. The authors concluded that “only methylcobalamin has a positive psychotropic alerting effect with a distribution of the sleep-wake cycle toward sleep reduction.”
More cases
Here’s a case of a 13 year-old boy with adrenoleukodystrophy who developed a sleep-wake disorder after a complete loss of vision. His sleep-wake cycle had been 25 hours, but normalized after taking methyl B12, which caused his plasma melatonin and beta-endorphin levels to more or less match those of healthy volunteers. His peak cortisol time shifted backwards. We also saw a case where methyl B12 successfully treated a 32 year-old man suffering from recurrent hypersomnia for 12 years.
Here’s another interesting case:
Two adolescent patients suffering from persistent sleep-wake schedule disorders appear to have responded to treatment with vitamin B12 (methylcobalamin). A 15-year-old girl with delayed sleep phase syndrome (DSPS) and a 17-year-old boy with hypernychthemeral syndrome complained of not being able to attend school despite many trials of medication. The improvement of the sleep-wake rhythm disorders appeared immediately after the administration of high doses (3,000 micrograms/day) of methylcobalamin. Neither patient showed any laboratory or clinical evidence of vitamin B12 deficiency or hypothyroidism (which can cause B12 deficiency). Serum concentrations of vitamin B12 during treatment were in the high range of normal or above normal.
Treatment of persistent sleep-wake schedule disorders in adolescents with methylcobalamin (vitamin B12)
Having issues with your sleep-wake schedule?
Then methyl B12 may help modulate your melatonin secretion, enhance your light sensitivity, and normalize your circadian and sleep-wake rhythm.
Any other benefits to methyl B12?
In one randomized study, 67 stroke patients received daily doses of 1500μg methyl B12, while 68 remained untreated. After two years, sensory nerve in the treated group was significantly improved compared to the untreated group.
Speaking of stroke, combining methyl B12 with folate is effective in reducing the risk of hip fractures in elderly patients following stroke. Add clonidine and moxonidine to the mix, and you improve baroreflex function in stroke-prone, hypertensive rats.
Some Chinese studies found methyl B12 helpful in lumbar disc herniation, thalamic pain, glaucoma, cervical spondylosis, and cubital tunnel syndrome. They also found acupoint methyl B12 shots with acupuncture to help against intractable facial paralysis.
Methyl B12 vs Cyano B12
Now, how does methylcobalamin compare to cyanocobalamin, the previous form we examined, when it comes to absorption and bio-availability?
Because of the effort needed to reduce cyano B12 to an active form, its absorption rate varies greatly between people. Generally, methyl B12 absorbs and retains in the body much better. It is so potent even orally it may help treat pernicious anemia:
A 73-year-old Japanese man with Hashimoto’s disease and diabetes mellitus received regular medical checkups for type 2 diabetes care. Blood tests indicated macrocytic anemia. The laboratory data demonstrated a normal folic acid level with a low vitamin B12 level. An endoscopic examination indicated no signs of gastric or intestinal bleeding. Positive results for anti-intrinsic factor antibodies were strongly suggestive of pernicious anemia. The patient refused cobalamin injections to treat the anemia. However, the oral administration of mecobalamin for the treatment of diabetic neuropathy was simultaneously initiated. Subsequently, the anemia gradually improved. Oral mecobalamin was presumably effective for pernicious anemia management.
Mecobalamin improved pernicious anemia in an elderly individual with Hashimoto’s disease and diabetes mellitus
Of course, we’re not suggesting you treat PA with oral tablets. Injections should always be the treatment (their absorption is far superior, and with PA you can’t take risks). But it still goes to show you the power of methyl B12 among all vitamin B12 forms.
For most people, methylcobalamin really is the best type of B12. If you can’t convince your doctor to prescribe it, we made it available to order here:
Hydroxocobalamin
(Also known as Hydroxycobalamin, Hydroxo B12, OH-Cbl, or B12a)
Hydroxocobalamin, a predominant form in B12 rich foods, is an inactive type of B12. Its benefit over cyano B12 is that it doesn’t have the toxic cyanide donor, so you bypass the need for detoxification and get to preserve the glutathione source.
Compared to cyano B12, it has a higher affinity to plasma protein and a longer half-life, retaining longer in the blood. This may help reduce B12 injection frequency.
Like cyano B12, hydroxo B12 has to convert in the body to either methyl B12 or adenosyl B12. It converts much easier, though. Cyano B12 doesn’t react easily to anything (the cyanide makes it very stable), so the body must expend energy for it to convert.
Actually, when you take methyl B12, a good amount converts to hydroxo B12 as soon as it donates its methyl group. Then, it has to receive another methyl group if your body ever wants to convert and use it as active vitamin B12.
Hydroxo B12 reacts chemically with cyanide, nitric oxide, and nitrous oxide. In fact, this form is common as an antidote for cyanide toxicity. Therefore, anybody can use it safely in tobacco amblyopia or in pernicious anemia with optic neuropathy. It’s also useful for patients with cobalamin metabolic diseases. But careful:
Suppressing NO (nitric oxide) can have adverse affects like elevated blood pressure, digestive disturbances, impotence, susceptibility to infection, and even increased risk of cancer. This is especially true during pregnancy, where NO helps control the feto-lacental circulation. Therefore, you’re better off with methyl or adenosyl B12.
Adenosylcobalamin
(Aka Adenosyl B12, AdeCbl, Cobamamide, Cobinamide, Dibencozide, or AdoB12)
Adenosylcobalamin is the mitochondrial form of B12. The enzyme methylmalonyl-CoA mutase uses it to convert methylmalonyl-CoA to succinylcholine CoA (in the synthesis of porphyrin). This is why methylmalonic acid (MMA) levels get high when you’re low on adenosyl B12. It also acts as an intermediate in the pathway for valine, threonine, methionine, thymine, isoleucine, cholesterol and odd-chain fatty acids.
Actuallly, our body stores most of our B12 reserves in the liver as adenosyl B12, and converts it to methyl B12 whenever needed.
But what about supplementing with adenosyl B12?
In one study, carnitine and adenosylcobalamin promoted cerebral mass growth, pyramidal neuron volume, neocortical layer thickness, and the restored normal structure of the neocortex in a model of anorexia nervosa. In the patients, carnitine and adenosyl B12 accelerated body-weight gain and gastrointestinal function normalization. Latent fatigue was gone and mental performance sharply increased.
Speaking of anorexia, another study found that the combined use of carnitine and adenosyl B12 eliminated fluctuations in work rate, and normalized the scope and productivity of intellectual work in patients with anorexia nervosa in the stage of cachexia. In this study, though, latent fatigue wasn’t fully gone.
An Italian study treated 37 persons suffering from viral hepatitis with either adenosyl B12 or cyano B12. The authors found adenosyl B12 to be significantly better than cyano B12 in normalizing total bilirubin, serum glutamic oxaloacetic transaminase (SGOT), serum glutamic pyruvic transaminase (SGPT), and alkaline phosphatase values.
Overall, 13 out of 18 of subjects who received the adenosyl B12 had their total bilirubin normalized, 15/18 had their SGOT normalized, 10/18 had their SGPT normalized, and 18/18 (all subjects) had their alkaline phosphatase normalized.
Not bad.
Adenosyl B12 vs methyl B12
So, which one is better for you?
Remember – these two B12 forms inter-convert in the body. The main benefit of methyl B12 over adenosyl B12 is that it comes with the methyl donor, further enhancing your health in a myriad of ways. Also, adenosyl B12 isn’t widely available in injectable form, and many people can only absorb B12 when it’s injected. However, if you can absorb B12 through the stomach, adenosyl B12 tablets can be a great option.
If your chronic fatigue seems to get better only with adenosyl B12 (and not with methyl B12), it’s possible that you have some rare condition preventing your body from the inter-conversion. In this case, use a mixture of both methyl B12 and adenosyl B12.
Verdict: Best Forms of Vitamin B12
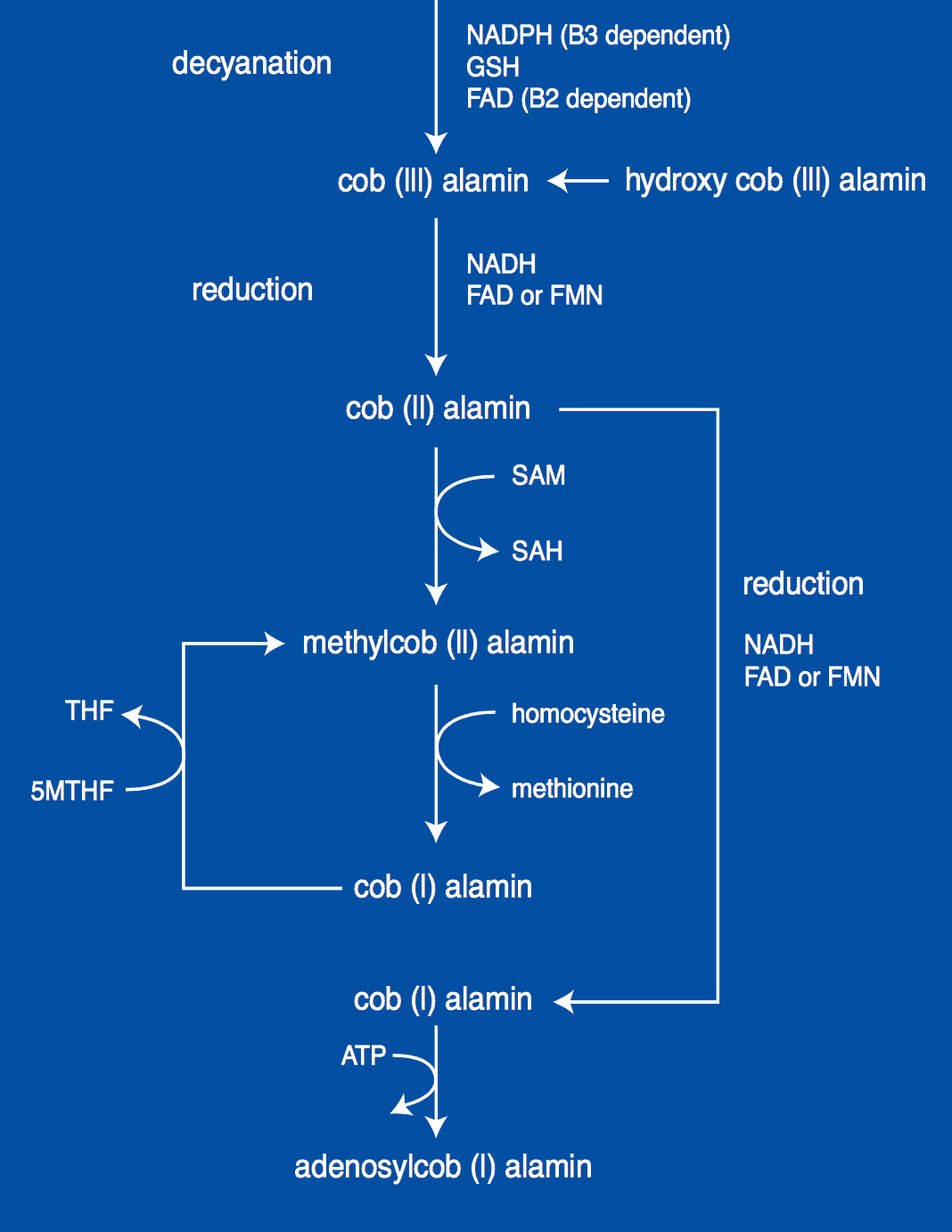
As you must have realized by now, some types of B12 are better than others. To try to visually grasp why the differences happen, here’s a good chart from George Kelly’s work, titled “On the synthesis of coenzyme forms of B12”:
So, which is the best type of B12?
Let’s wrap things up.
Cyano B12 is an inactive, slightly toxic form of B12. It contains a cyanide molecule, which your body will have to remove through methylation, a reaction that requires methyl groups. Glutathione seems to be the agent performing the decyanation. Only then can the cobalt atom be reduced from an oxidative state of +3 to the biologically active +1, forming methyl B12 in the cytosol, and adenosyl B12 in the mitochondria. This conversion is demanding, and can be compromised in a range of conditions.
Cyano B12 is especially risky to those with liver problems, renal failure, and smokers, because in these people the cyanide can’t be cleared out properly. It’s also dangerous for pernicious anemia patients or anyone with high homocysteine levels, because it may deplete the body of glutathione, a substance needed to lower homocysteine.
As a result, we recommend this form to absolutely no one.
Hydroxo B12 is an inactive form of B12 as well, but it is much better than cyano B12. This is because it doesn’t contain cyanide, thus bypassing the need for decyanation and preserving the glutathione. Just like cyanocobalamin, it has to be reduced from state +3 to +1 before it can become either methyl B12 or adenosyl B12.
We recommend this form to B12 deficiency patients with tobacco amblyopia, cyanide toxicity, and/or early hereditary optic nerve atrophy (Leber’s disease). Remember to always monitor nitric oxide levels during administration. However, if you can get methyl or adenosyl B12 instead, do that. It is always the better route.
And so, the best vitamin B12 forms are…
Adenosyl B12 and methyl B12 are the native forms of vitamin B12, bypassing several steps in the absorption cycle. Both of them absorb, retain, and increase tissue concentration much better. As a result, they often produce clinical results far superior to what either cyano or hydroxo B12 can offer. Their use offers significant benefits and should be the first line of defense against conditions that may benefit from B12.
But, if you had to choose, which of them is the superior choice?
Remember, these two forms of vitamin B12 inter-convert. If you have a rare condition that prevents this conversion, you’ll have to use a combination of both.
For most people, however, methyl B12 is enough, and the best choice for recovery. It shows distinct neuroprotective effects, as it improves nerve regeneration and brings synaptic transmutations and diminished neurotransmitters back to normal levels.
Unlike adenosyl B12, methyl B12 donates a valuable methyl group that further enhances your health (unlike cyano, which steals one). This is especially important for pernicious anemia patients or anyone suffering from high homocysteine levels. This donation of methyl groups may be the reason why methyl B12 is so helpful in many conditions.
Methyl B12 simply solves the most problems simultaneously.
It’s our favorite form.