How to test for B12 levels properly and determine whether or not you suffer from a deficiency of B12? Unfortunately, many B12 deficiency cases are discovered too late, or worse, are entirely missed. Doctors often misdiagnose it as some other condition, and as a result patients end up with lifelong neurological damage that could have been easily prevented if caught on time. Therefore, the early diagnosis of B12 deficiency is crucial, and you should make sure your doctor is performing the process properly.

Vitamin B12 Deficiency Diagnosis Issues
First, a word on the all-too-common issue of misdiagnosis. When vitamin B12 deficiency starts to affect the nerves, doctors tend to misdiagnose it as some other illness with similar symptoms, or blame a co-existing condition which may actually be the result of the B12 deficiency. Some of these conditions and illnesses could be:
- Parkinson’s
- Alzheimer’s
- Multiple sclerosis
- Autism
- Bipolar disorder
- ADHD
- Diabetic neuropathy
- Vertigo
- Chronic fatigue syndrome
- Chronic pain disorder
- Psychosis
- Functional neurological disorder
- Schizophrenia
- Depression
- Fibromyalgia
- Myalgic encephalomyelitis
- Mini-strokes
- Crohn’s
- Irritable bowel syndrome
- Optic neuritis
- Folate deficiency
- Infertility
- Hypothyroidism
Why is misdiagnosis so common?
- Extremely poor knowledge among doctors, leading to symptomatic people not being tested at all. Often, a patient complaining about depression will be prescribed antidepressants instead of being tested for B12 deficiency. Doctors just do not think to test for B12 deficiency, and in most countries you have to ask your doctor to do it. Health care professionals simply assume meat eaters get enough B12 from their diet, so they don’t even bother to check for B12 deficiency. However, most cases of a lack of B12 are the result of malabsorption, rather than low consumption.
- Even when doctors do test for B12 deficiency, there are some major problems with the regular blood test, as you’ll see in a moment.
- Before testing for B12 levels, doctors often look for macrocytosis (enlarged red blood cells), but this is the last, advanced stage of B12 deficiency. Only about 60% of B12 deficiency patients are macrocytic, and at that point some of the damage can’t be reversed. Even neurological signs and symptoms – which indicate severe B12 deficiency – may be present despite having normal red blood cells.
- Doctors tend to assume that the neurological effects of B12 deficiency, like tremors, falling, or cognitive decline, are all part of the normal process of aging. Thus, elderly people, who are at the highest risk of B12 deficiency, aren’t even tested. Sometimes, they don’t blame the symptoms on aging, but rather on other co-existing medical conditions. Similarly, mental health patients and pregnant or breastfeeding women, groups who are at real risk of B12 deficiency, aren’t tested either.
- It is probable that research simply tends to gravitate towards where the potential for profit is. Simply put, there’s more money to be made treating B12 deficiencies with the resulting neurological damage that demands complex medicines, rather than preventing them in the first place. It’s only natural that research funds would go that direction, leading doctors to being so unbelievably misinformed.
Vitamin B12 Deficiency Tests
So, how do you test for B12 deficiency properly? Here are all the tests available, and how effective they are. Let’s start with the most common B12 blood test:
Total-B12 Blood Test
Total serum or plasma cobalamin measurement is the most common blood test for B12. In other words, it is the standard front-line clinical test for vitamin B12 deficiency. Which, by the way, is a very unfortunate situation, because the test is far from accurate. The total-B12 test suffers from a number of serious limitations:
- It measures all circulating B12, not distinguishing active B12 (transcobalamin II) from unusable, inactive analogues (transcobalamin I and III). Inactive B12 may represent as much as 90% of your total levels. So, even if your results are within the normal range, you may still be deficient if a large portion of your B12 is inactive. Imagine looking at a fuel gauge of a petrol car, indicating the tank is full. However, if the tank was topped up with diesel, the engine would come to shuddering halt.
- False positives and negatives. For example, total B12 levels of less than 148pmol/L (200pg/mL) are considered indicative of deficiency. However, some individuals with levels below this cut-off exhibit no clinical or biochemical evidence of deficiency. It was shown that low haptocorrin levels (leading to low levels of inactive B12) are likely to be the one of the most common causes of low total-B12 levels. Conversely, neuropsychiatric and metabolic abnormalities can happen with plasma B12 levels well within the normal reference interval. In fact, around 50% of B12 deficiency cases are not detected when the B12 test is used with a 148pmol/L cut-off.
It’s also possible that a person could be suffering from B12 deficiency even though his B12 blood test shows a very high number. Conditions such as liver disease or cell death (for example, due to cancer, which breaks down tissues), may release B12 back into the blood circulation, tricking the test into thinking B12 stores are large.
Many papers attest to a significant gray zone when using the total-B12 test: Snow suggests total-B12 assays discriminate poorly at levels of 75-300 pmol/l. Swain suggests that levels of 150-300 pmol/l require confirmation. Hvas and colleagues recommend further testing when B12 levels are 125-250 pmol/l. Schneede suggests follow-up testing when B12 values are 150-250 pmol/l. Klee suggests follow-up testing when B12 is 110-220 pmol/l. Herrmann estimates B12 deficiency can occur even in B12 levels of 300pmol/L, and that 45% of B12 deficient subjects would be overlooked if their doctor only relied on total-B12 as a screening test.
- Late marker. Active B12 has a shorter circulating half-life compared to inactive B12, so the earliest change that occurs on entering negative B12 balance (low total-B12 levels) is likely to be a decrease in plasma active B12 (holoTC) concentration.
- The normal B12 level range is too low. Some countries accept levels as low as 100. As a result, doctors often miss and refuse to treat desperately deficient patients, even when they show obvious symptoms. These doctors should know that B12 deficiency begins to appear in the cerebrospinal fluid below blood levels of 550. Why would being diagnosed with B12 deficiency depend on your geography?
- The typical B12 test uses a competitive binding luminescence assay. It gives false high results in 22-35% of patients, depending on the machine.
In short, it has become clear that the total serum vitamin B12 level test may be misleading. It doesn’t tell you the whole story, and is often not congruent at all with what’s happening at the cellular level, where it actually matters. Other B12 deficiency diagnostic tests currently used to assess B12 status are active B12, methylmalonic acid (MMA) and, less commonly, total homocysteine (tHcy). Let’s explore them.
Active-B12 Test (HoloTC, or Holotranscobalamin II)
One of the best tests is holoTC (holotranscobalamin II), because it only measures levels of functional, active B12 in the blood. We predict that it will one day replace the regular test entirely, because there are often big gaps between the total levels of B12 and those of active B12. This test should be a first-line diagnostic tool, as low levels may point to B12 depletion at the cellular level. Unfortunately, most hospitals don’t offer this test.
We’re big fans of this test. You can do it privately at Viapath.
MMA Test (Methylmalonic Acid)
MMA is high in around 95% of B12 deficiency cases.
One of the core functions of vitamin B12 is converting methylmalonyl-CoA – a thioester consisting of coenzyme A linked to MMA – into succinyl-CoA. Therefore, when you’re deficient in B12, your MMA levels will increase in your blood and urine.
The MMA test is a phenomenal test, but it’s not very popular, because it uses the expensive gas chromatography mass spectrometry (GC-MS). You may be able to order an MMA test as a follow-up to a blood test showing B12 in the lower end of the normal range. In such a case, having high MMA levels will be confirmatory.
If you can’t get your doctor to prescribe an MMA test, you can order a uMMA (urinary MMA) test directly from its founder, Dr. Eric Norman. This version is even better, because B12 deficient patients with neurological damage excrete significantly more uMMA than those without. Therefore, a uMMA test can predict your path toward lifelong neurological damage. The test has an impressive 99% accuracy, making it confirmatory.
However, false high levels of blood MMA (or false low levels of uMMA) could result from renal failure, because it’s the kidney’s job to flush out the MMA. Other possible causes of high serum levels could be intestinal bacterial overgrowth, hemoconcentration, thyroid disease, pregnancy, or a rare genetic disorder called methylmalonic acidemia. There is also the possibility that some pathways have greater or lesser priority. For example, high serum MMA levels in healthy folks with B12 levels at the high end of the normal range might suggest that supplying cobalamin to MMA-CoA mutase has a low priority.
How do you interpret an MMA test results?
For the serum MMA test, anything higher than 0.40nmol/mL indicates a B12 deficiency. Even in the presence of confounding factors, if plasma levels surpass 0.75 nmol/mL, it’s most likely a B12 deficiency. As for the uMMA test, units are different, and anything higher than 3.60mmol MMA/mol creatinine points to a deficiency.
Do note, your MMA levels do not necessarily reflect the stage of your B12 deficiency, and there may also be a high variation in MMA levels when measured over time.
Total-Homocysteine Test (tHcy)
The body uses methylcobalamin, one of the native B12 forms, to convert homocysteine back into methionine. Therefore, the homocysteine test is an extra tool to determine your true B12 status. Even if your B12 blood levels look normal, high homocysteine levels may indicate a functional deficiency or a decreased capacity to utilize methyl B12.
This is double as true when the typical symptoms of B12 deficiency are present. Just like the MMA test, the tHCY test may provide information on functional intracellular B12 homeostasis, regardless of the underlying reasons for deficiency.
Do note, however, that high homocysteine levels may be high even in the face of normal B12 status. This may be the result of low B6 or folate, renal failure, hypothyroidism, an enzymatic dysfunction in the methylation cycle, or reasons not fully elucidated.
Also, the total-homocysteine test must also be carried out within two hours of sampling the blood, which must be cooled during that time.
What’s The Best Vitamin B12 Test?
By now it’s become pretty obvious how misleading the total-B12 blood test can be. As for tHcy and MMA, studies have shown that both levels may increase with age, as high levels are common among the elderly, even among supposedly healthy old people. Research has suggested that only about 17% of the variation in MMA levels between a middle aged and an elderly group could be accounted for by B12 and kidney function. In other words, the determinants of MMA levels in an elderly population are largely unknown.
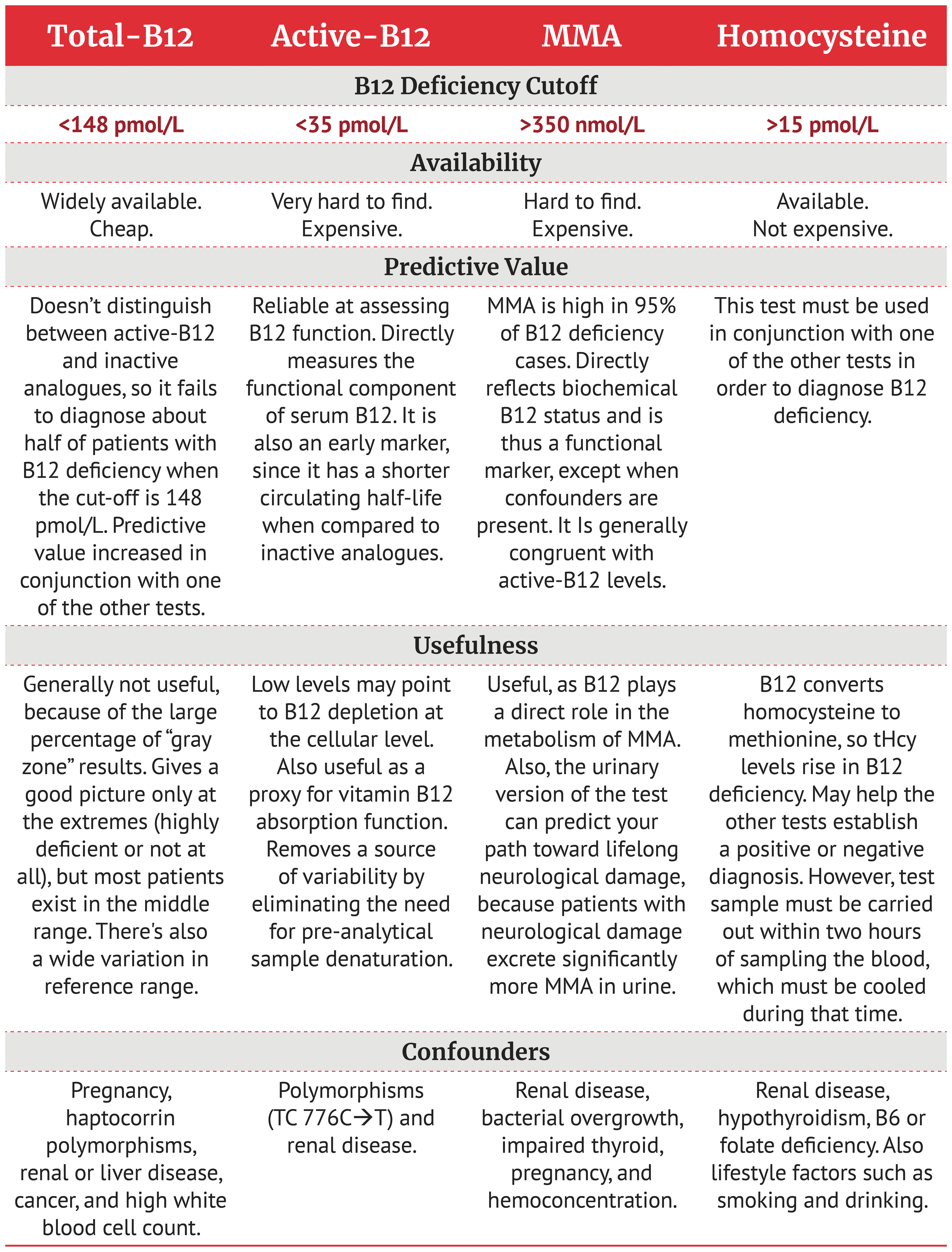
That being said, the MMA test is very useful most of the time. It directly reflects biochemical B12 status, except when confounders are present. Our affinity for it is surpassed only by our fondness for the active-B12 test, which measures the functional part of serum B12 directly. Here’s a summary of the pros and cons of each test:
Other B12 Deficiency Tests
MCH / MCHC
Testing for MCH (mean corpuscular hemoglobin) will reveal how much hemoglobin you have per red blood cell. Testing for MCHC (mean corpuscular hemoglobin concentration) will also account for the cell volume. High levels in any of these two tests may indicate a B12 deficiency. They’re not conclusive, but can be used as an extra tool.
Pepsinogen I & Gastrin
Once B12 deficiency has been diagnosed, the next challenge is to find the cause (unless obviously dietary). There are a number of markers for estimating the function of the gastric mucosa. Two such tests are serum gastrin and serum pepsinogen I. Low serum pepsinogen I indicates extensive atrophy of the gastric mucosa.
However, pepsinogen I levels can rise in superficial gastritis, as observed in H. pylori infections. High serum gastrin levels generally indicate atrophy in the corpus and fundus of the stomach, but may also be caused by a gastrin-producing tumor. Like pepsinogen I, the specificity of this marker for B12 deficiency is low.
The Shilling Test
The Schilling test was diagnosing a lack of intrinsic factor, finding out if you have true pernicious anemia. It was used to discover the cause of your B12 deficiency – whether you can absorb B12 normally or not, and if not, then why – after deficiency had already been confirmed. Thus, it was also called the “vitamin B12 absorption test”.
However, patients with gastritis and B12 malabsorption due to an inability to break down the protein-B12 complex in the food may get normal tests results. The test is rarely used. It is considered obsolete and is no longer available at most medical centers.
You’re very unlikely to find it, but there’s no need to. B12 shots are inexpensive, safe, and are the preferred treatment for most B12 deficiency cases anyway.
Who Should You Test For B12?
By default, health care professionals should test anybody who shows even the slightest symptoms of B12 deficiency or pernicious anemia. Treatment is easy, and can prevent lifelong damage. Here are the groups at the highest risk of B12 deficiency:
- The elderly. 20-30% of people above age of 50 develop atrophic gastritis, a disease in which B12 absorption is impaired. This is confirmed by numerous studies.
- Kids with developmental delays. It can take years before B12 deficiency develops in adults, because our body stores B12 for future use. Children, in contrast, don’t have the rich stores adults have, and can develop deficiency quickly.
- Pregnant and breastfeeding women. Fetuses and breast-fed infants drain nutrients from their mothers. These women should be taking extra B12.
- Women with post-natal depression or a history of infertility or miscarriages. These women should be tested immediately for B12 deficiency.
- Vegetarians and vegans. Every vegetarian should supplement with B12. Up to 80% of long-term vegans are B12 deficient. Do not take this lightly.
- Gastrointestinal surgery patients. If you had any surgery where any part of your stomach or ileum was removed – including surgeries for weight loss purposes – you’re likely to need a lot more B12 than before.
- People on certain medications. This includes proton pump inhibitors, H2 blockers, antacids, metformin, or any other medication which can interfere with B12 absorption. Those undergoing chemotherapy or using nitrous oxide (laughing gas) regularly should also be supplementing with B12.
- Anyone with gastrointestinal diseases. Anyone diagnosed with a disease that may lead to malabsorption of nutrients, for example Crohn’s, ulcerative colitis, irritable bowel syndrome, and celiac. Also, misdiagnosis is common. We recently had a woman come to us with an unresolved Crohn’s. She’s been on medication for years. Turns out, she never had Crohn’s. She had B12 deficiency, because our B12 shots combined with our diet led to 100% remission in her symptoms.
- Heavy smokers or alcoholics. Toxins may deplete B12 stores.
- People with a history of eating disorders.
- Anemic people.
How to Diagnose B12 Deficiency?
So, how do you diagnose B12 deficiency correctly? As you saw, it’s not as straightforward as simply looking at the total-B12 blood test, because it’s not reliable enough. You can have very high numbers of B12 in the blood and still be deficient.
The active-B12 test would be our immediate go-to. But it’s not so easy to find, and in many places impossible. That leaves us with the MMA and homocysteine tests.
As for homocysteine, levels may rise not just in the absence of B12, but in the absence of B6 and folate as well. Likewise, MMA may rise in the presence of kidney failure, thyroid disease, intestinal bacterial overgrowth, and a few more conditions.
So, what do you do?
The obvious option is to combine them. If both your MMA and homocysteine levels are high, then you’re likely suffering from B12 deficiency. However, If homocysteine (but not MMA) levels are elevated, then you may actually have folate deficiency. If both MMA and homocysteine levels are fine, chances for B12 deficiency are slim.
Regardless, if your total-B12 levels are extremely low, you likely suffer from a deficiency of B12. If you do Dr. Eric Norman’s uMMA test and get high results, you almost certainly suffer from B12 deficiency. High uMMA levels are as confirmatory as it gets.
Important:
We highly recommend to test for folate (B9), ferritin (iron storage), and to do a full blood count. This is because B12 and folate need each other, and optimal levels of iron are just as important as optimal B12 levels.
Also, before having any vitamin B12 deficiency test, do NOT supplement with B12 for at least 72 hours, because it could skew your results. Some labs may prefer not to draw a blood sample within two weeks of a B12 injection.
If you suspect your B12 deficiency is the result of pernicious anemia, go do the necessary tests, which will test for specific antibodies. Even in the absence of anemia, unexplained low levels of B12 should be tested for PA.
Symptoms Above Biomarkers
This brings us to the central point. Perhaps the primary question should be, how obvious are your B12 deficiency or pernicious anemia symptoms?
To quote NEQAS:
In the event of any discordance between clinical findings of B12 deficiency and a normal B12 laboratory result, then treatment should not be delayed. Clinical findings might include possible pernicious anaemia or neuropathy including subacute combined degeneration of the cord. We recommend storing serum for further analysis including MMA, or holotranscobalamin and intrinsic factor antibody analysis, and treating the patient immediately with parenteral B12 treatment.
THE UNITED KINGDOM NATIONAL QUALITY ASSESSMENT SCHEME FOR HAEMATINIC ASSAYS
As you can see, the NEQAS recommends to look at the clinical picture, and give patients B12 injections based on their symptoms alone. This is because the risks of delaying treatment while waiting for B12 deficiency diagnosis, disproportionally outweigh the benefits of taking action. The message is, if you show clear symptoms of B12 deficiency, start injecting B12 right away. Ask your doctor for a trial of methylcobalamin B12 shots. If they refuse, you can buy injectable B12 here and take control of your health.
Remember, vitamin B12 has no toxicity levels, and you can’t overdose. There is no risk. Anything your body doesn’t need goes out through the urine in hours. So, if you show clear symptoms, don’t put off treatment waiting for diagnosis. Start injecting.
If you suspect you may be suffering from B12 deficiency, then take action now. Disregard blood levels of B12 and go by symptoms alone. There’s a short window of opportunity for effective intervention, especially to those with nerve-related symptoms. The risk is too high. Wait long enough, and you end up with severe, lifelong neurological damage, because the myelin sheath around your nerves gradually strips off.
In such cases, B12 shots are the quickest way to avoid major nerve damage. Injecting B12 early may save your nerve system, life quality, and sanity. We recommend to inject daily, for at least three months, and then gauge improvement. If you feel much better than before, you’re very likely to have suffered from B12 deficiency. Keep injecting until you sort it out. If it’s pernicious anemia, you’ll likely have to inject for life. If not, then injecting may be temporary, until you find the root cause and treat it.
Best of luck.